Engorgement
More than mild engorgement in the breasts is usually a sign that the breastfeeding is not going very well. It is due to the combination of milk stasis (the milk is not coming out) and oedema (swelling due to water retention in the area). Severe engorgement about the third or fourth day after the baby is born can usually be prevented by getting the baby latched on well and drinking well from the very beginning. See the information sheets Starting out right and The importance of skin-to-skin contact, and Increase intake of breastmilk. See also ibconline.ca for videos to help use the Protocol for Managing Breastmilk Intake. If you do become engorged, please understand that engorgement goes away within 1 or 2 days even without any treatment, but can be uncomfortable during that time. Massaging the breasts in a downward motion is not recommended as a treatment for engorgement. Continue to breastfeed the baby, making sure he gets on well and nurses well and the engorgement will resolve. However, if you should get engorged to the point where the baby is not able to take the breast, or if there is more than minimal discomfort in the breast and/or areola (the coloured part surrounding the nipple), then there is a simple way to temporarily move swelling away from the areola:
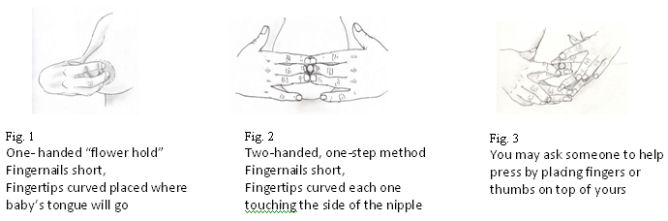
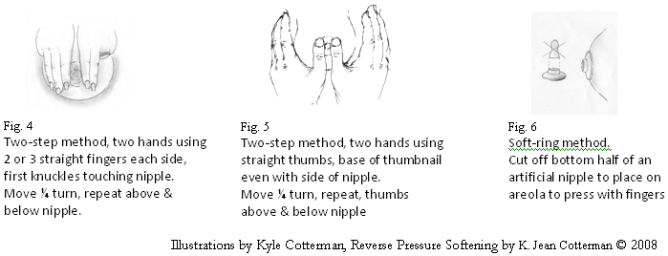
How to do REVERSE PRESSURE SOFTENING
Developed by K. Jean Cotterman RNC-E, IBCLC
Try this if pain, swelling, or fullness creates problems during the early days of learning to breastfeed. The key is making the areola very soft right around the base of the nipple, for better latching.
- A softer areola protects the nipple deep in baby’s mouth helping his tongue remove milk better. Mothers say curved fingers work best. (Fig. 1 or 2)
- Press inward toward the chest wall and count slowly to 50.
- Pressure should be steady and firm, and gentle enough to avoid pain.
- If mom wishes, someone else may help, using thumbs (Fig. 5).
- (For long fingernails, try another way shown below.)
- If breasts are quite large or very swollen, count very slowly, with mom lying down on her back. This delays return of swelling to the areola, giving more time to latch.
- Soften the areola right before each feeding (or pumping) till swelling goes away. For some mothers, this takes 2-4 days.
- Make any pumping sessions short, with pauses to re-soften the areola if needed.
- Use medium or low vacuum, to reduce the return of swelling into the areola.
Cabbage Leaves and Compresses
Cabbage leaves may also be used to help decrease the engorgement, as can ice packs and cold compresses. Some studies suggest cabbage may accomplish this more quickly. If you are unable to get the baby latched on, start cabbage leaves, start expressing your milk, and give the expressed milk to the baby by spoon, cup, finger feeding or eyedropper and get help quickly. See also the information sheet When baby does not yet latch.
- Use green cabbage
- Crush the cabbage leaves with a rolling pin if the leaves do not take the shape of your breast.
- Wrap the cabbage leaves around the breast and leave on for about 20 minutes. Twice daily is enough. It is usual to use the cabbage leaf treatment less than two or three times. Some will say to use the cabbage leaves after each feeding and leave them on until they wilt. Some are concerned that using them too often will decrease the milk supply.
- Stop using as soon as engorgement is beginning to go away and you are becoming more comfortable.
- You can use acetaminophen (Tylenol™, others) with or without codeine, ibuprofen, or other medication for pain relief. As with almost all medications, there is no reason to stop breastfeeding when taking analgesics.
- Ice packs also can be helpful.
- Some women get a large lump in the armpit about 3 or 4 days after the baby’s birth. Cabbage leaves may be used in that area as well to help the lump go away.
Epsom salts
(Please note: We have not had much experience with this approach but have heard some good things about it. We include it to provide an alternative to the above). (This technique is adapted from handout Patient’s Treatment for Engorgement, by A. Stolz, with notes from Lawrence, R; Ingle, B; Hunt, A)
The breasts may be soaked in a tub or basin of epsom salts for a few minutes to help with engorgement.
- Fill a small container or basin with warm water, deep enough that the breast can be submerged (You may need about 1 litre of water, or more).
- Place 1–2 handfuls (what fits into the palm of the hand or about 30 to 60 grams), of Epsom’s salts crystals (magnesium sulphate, MgSO4) and dissolve before putting the breast in the water
- Mother can lean over the basin so her breasts soak in the solution
- This should not be painful and any cuts or trauma can be covered with All purpose nipple ointment
- Leave soaking in very warm water until water is cool or at least 5-10 minutes
- Wash off solution with plain water after, to wash away salty taste for baby
- The salts may act as a diuretic for excess fluids in the breast
- Repeat before each feed or 3 or more times a day as Mother wishes
- Usually good results can be felt in 24 hours
- Mother can do this treatment for up to 3 days if desired
Engorgement, Revised 2009
Written by Edith Kernerman, IBCLC, revised by Jack Newman, MD, FRCPC © 2009
Reverse Pressure Softening written by Jean Cotterman, illustrations by Kyle Cotterman, © 2008
Epsom Salt notes from A. Stolz
